Meet the SemaPen Ecosystem
A single, intuitive app combines onboarding, prescriptions, weight tracking and live clinician chat.
Backed by Phoenix Health’s two decades of bariatric expertise, SemaPen offers hospital‑grade governance in a consumer‑grade interface.
Data flow is seamless: Withings® smart scales sync to the cloud so clinicians can intervene early and personalise advice.
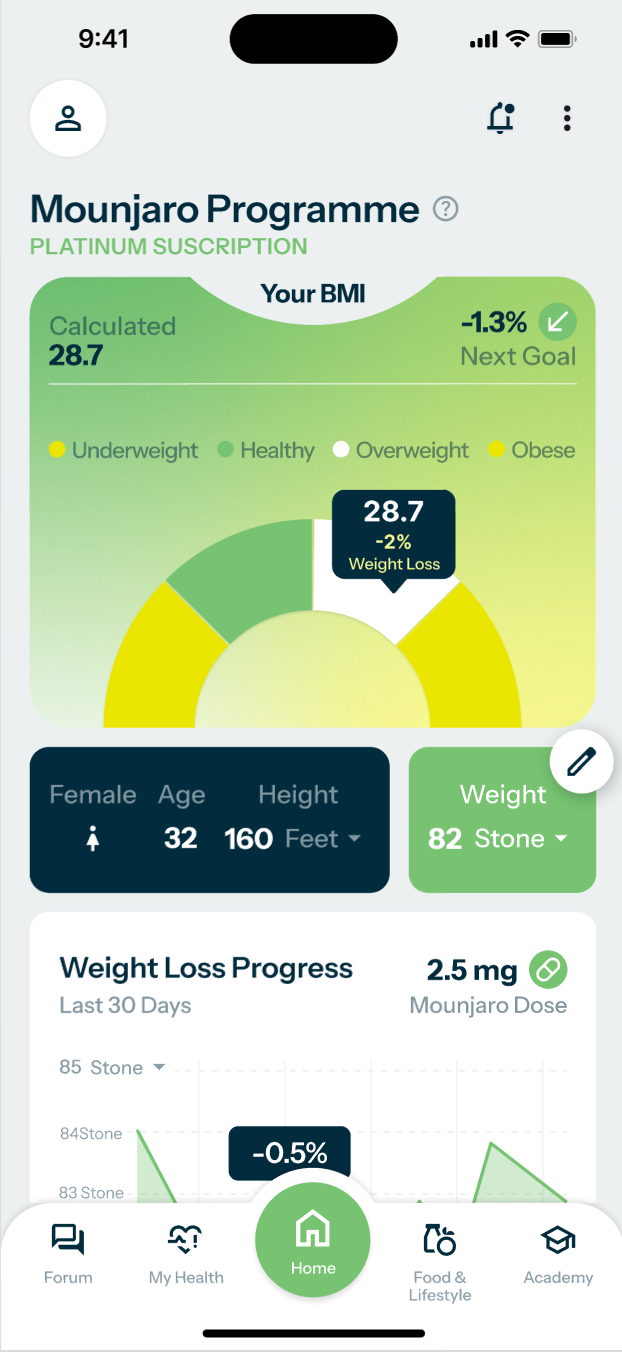
In‑App Dashboard
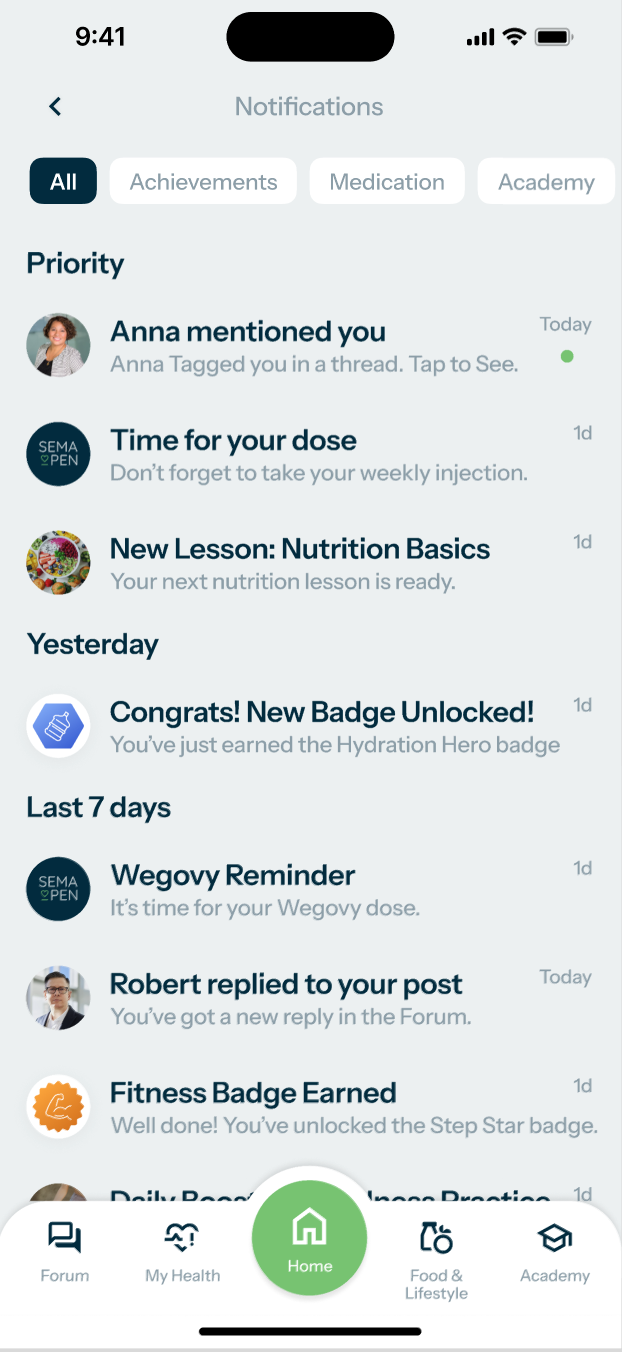
Patients open the app to an at‑a‑glance weight curve, BMI, weekly injection timer and goal streaks.
One‑tap access to secure messaging means questions are answered in hours, not weeks.
Automated nudges celebrate milestones and flag missed doses, increasing adherence without extra clinic time.
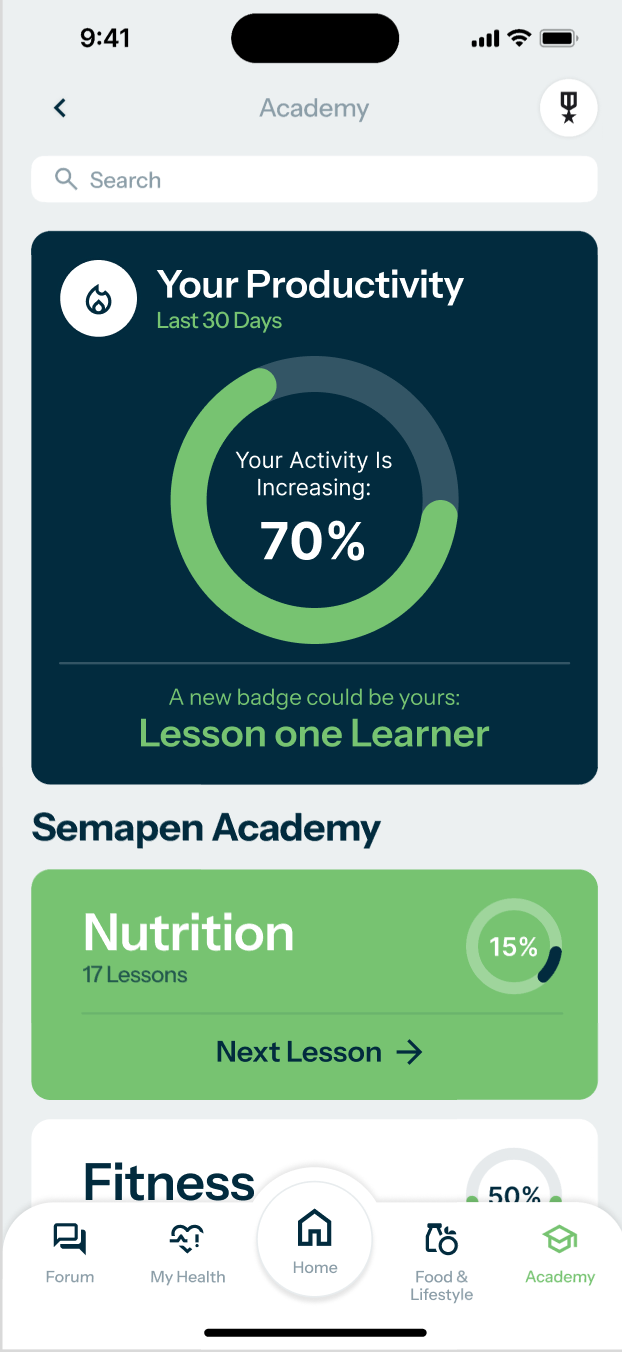
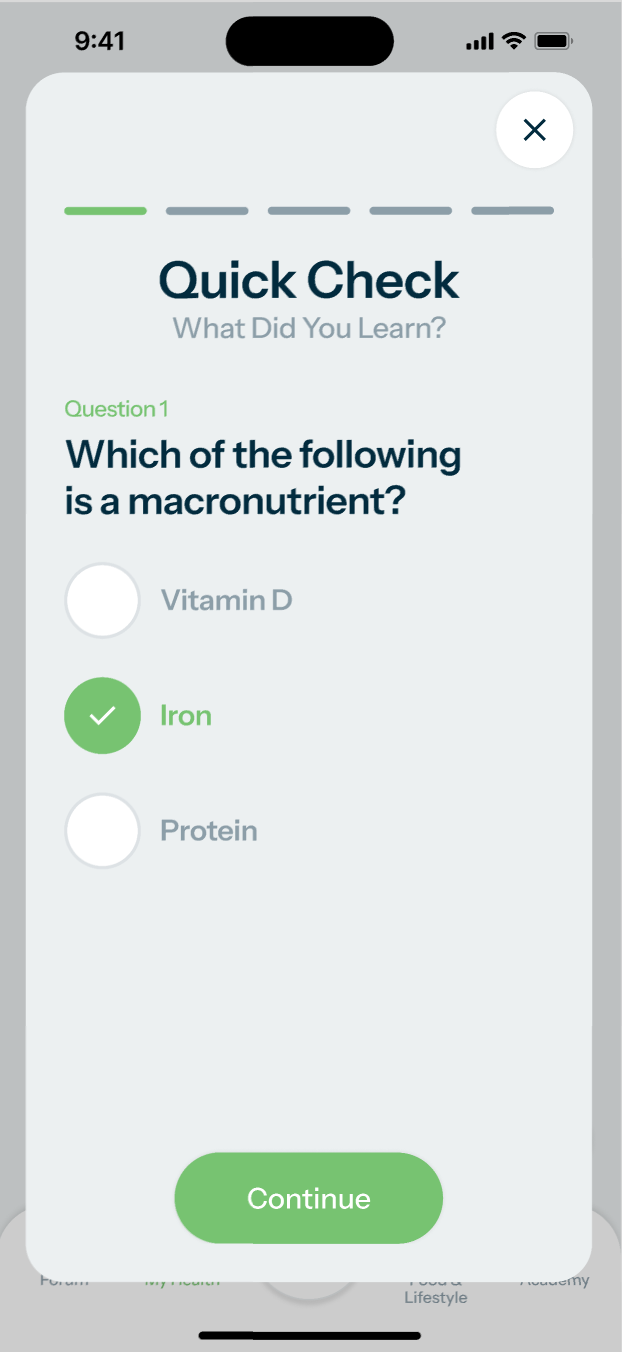
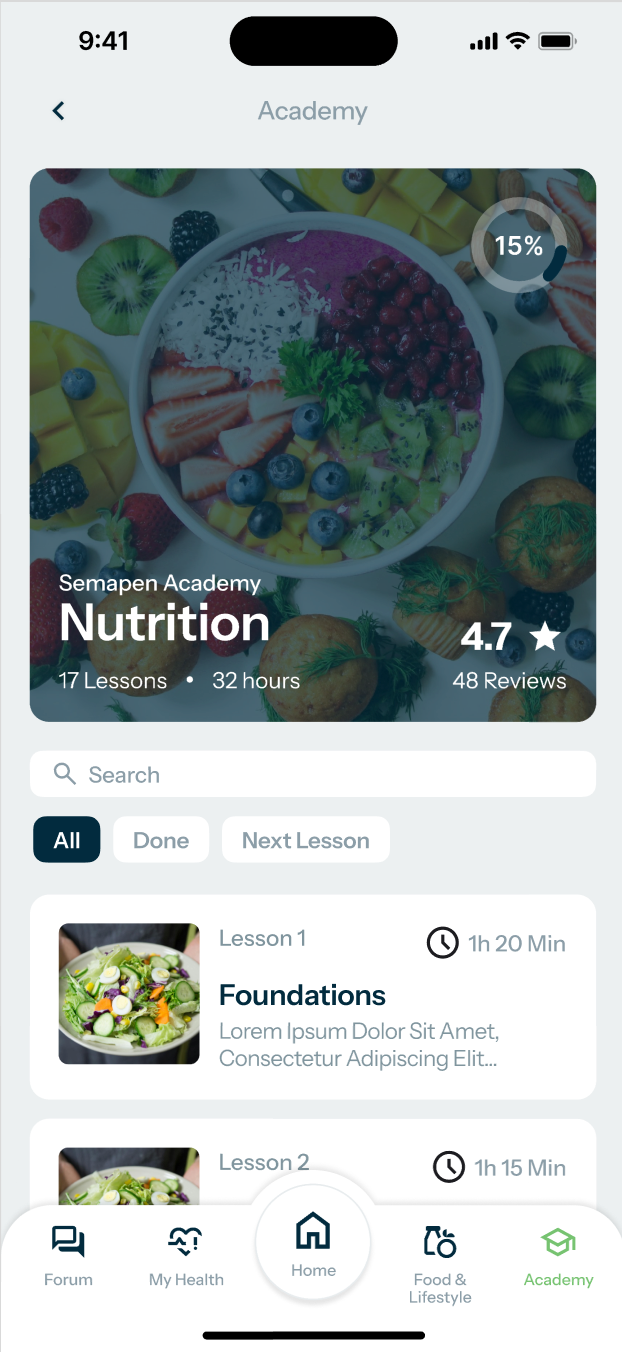
The Academy
Bite‑size lessons, quizzes and videos translate NHS guidelines into everyday habits.
New modules drop monthly under the maintenance contract, keeping content fresh and CPD‑aligned.
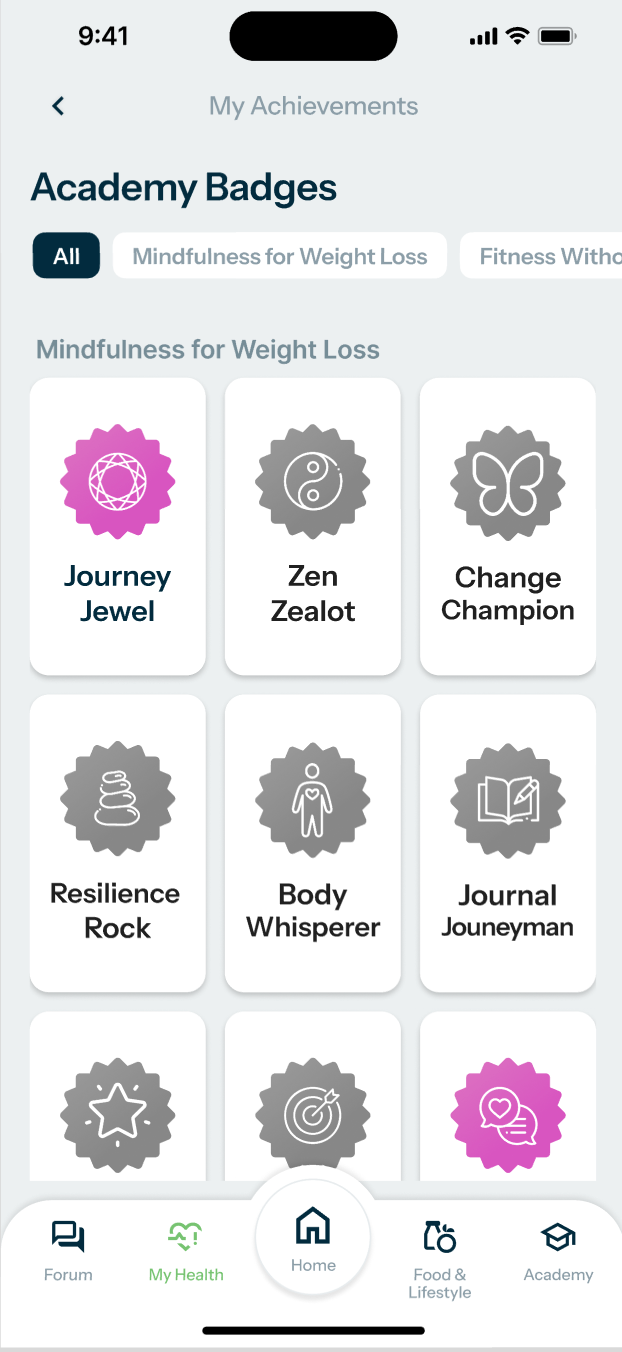
Completion badges gamify learning and contribute to the app’s reward system, driving regular log‑ins
Injection Programme
Once‑weekly Wegovy delivers ~15 % mean weight loss, while Mounjaro lifts that to ~21 %.
Clinical trials show more than 85 % of users shed at least 5 % body weight – the threshold for meaningful metabolic improvement.
SemaPen automates dosing escalation, side‑effect triage and drug delivery, freeing NHS staff for complex cases.
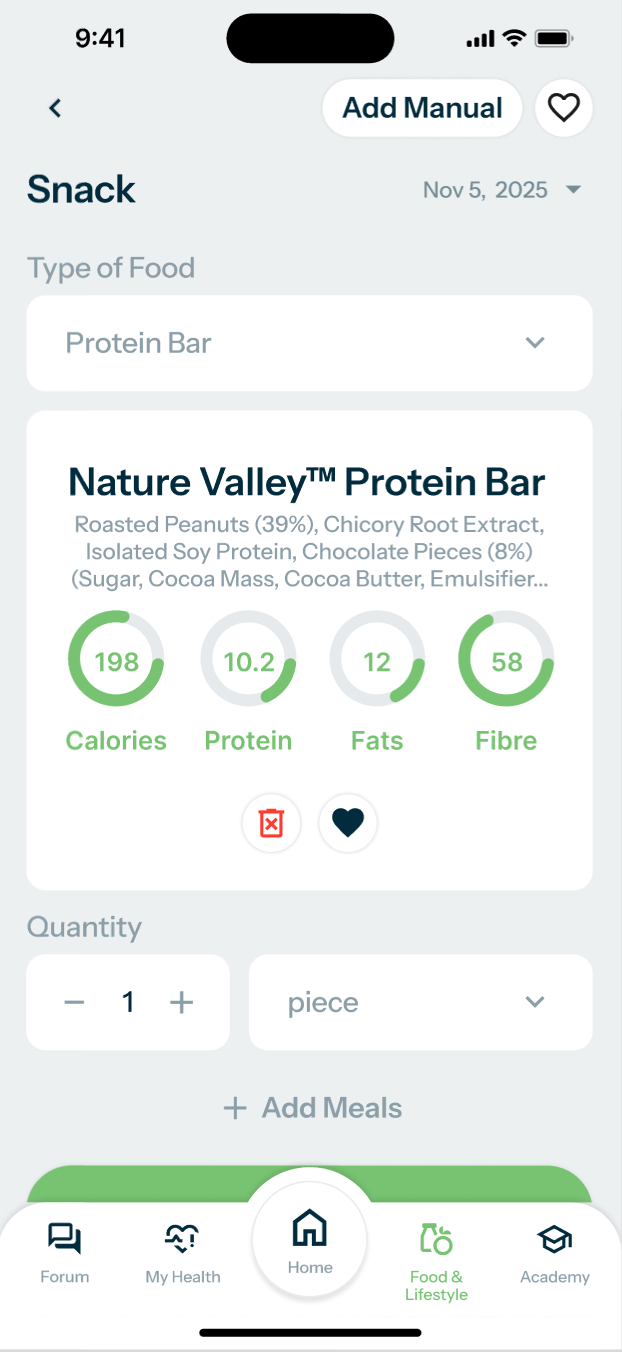
Nutrition‑Only Programme
Patients who prefer to avoid injections still enjoy the full SemaPen experience: dietitian‑designed meal plans, Academy learning modules and the same gamified dashboards that celebrate every healthy habit.
Smart meal‑logging (Phase 3 feature) analyses macros in real time and awards points for consistency, keeping motivation high.
Clinicians continue to monitor live weight data and symptom check‑ins, providing the same safety net—just without the prescription cost.
Benefits for the NHS
SemaPen scales nationally, giving millions of adults living with obesity a single, cost‑effective digital pathway.
Earlier weight reduction prevents progression to diabetes, cardiovascular and joint disease, easing long‑term pressure on clinics, theatres and prescribing budgets.
In‑app health check‑ins let patients record improvements in blood pressure, HbA1c, sleep apnoea and mood, creating a real‑world evidence loop commissioners can trust.
Benefits for Patients
Lose weight, keep it off: sustained results at 12 months with tailored lifestyle coaching and pharmacotherapy where appropriate.
No clinic queues: onboarding, prescriptions and check‑ins happen from the sofa, increasing access for rural and mobility‑limited users.
Holistic support – psychology, dietetics and peer community – tackles root behaviours, not just the scales.
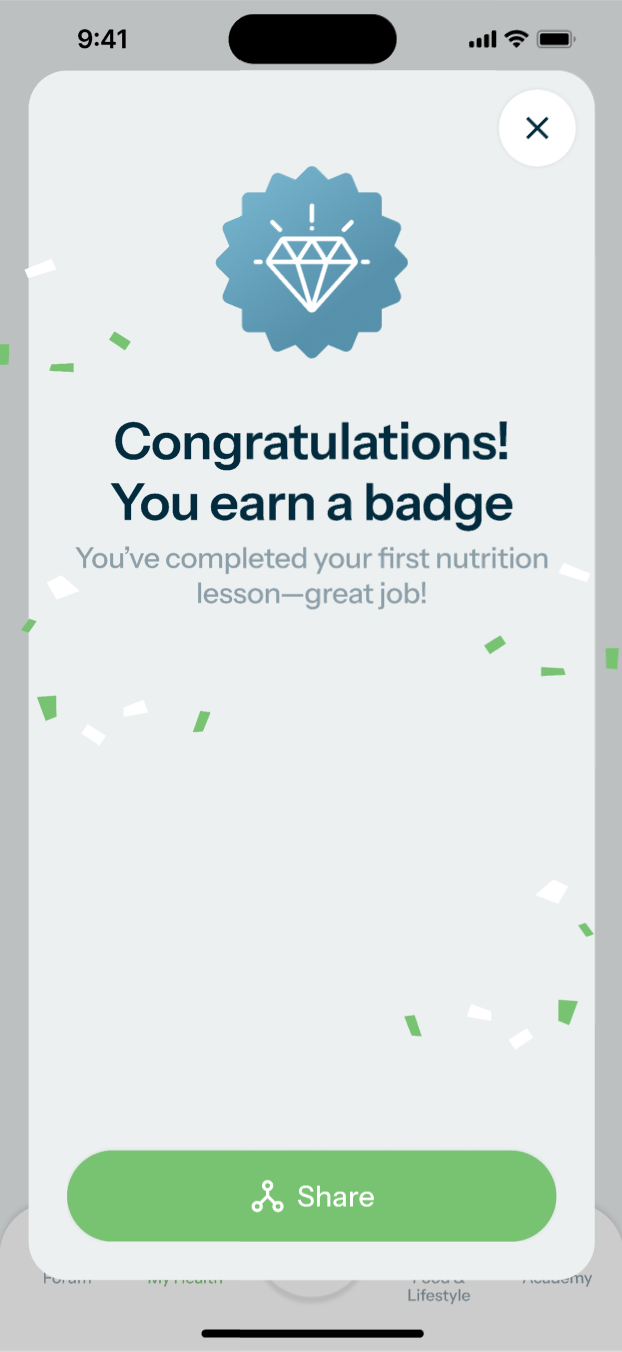
Congratulation! You earn a badge
Engagement Extras
Gamified dashboards—streaks, badges and leaderboards—turn healthy habits into a game, boosting daily log‑ins.
Weekly micro‑challenges and social sharing features foster friendly competition and peer support.
Push‑notification tips and celebratory animations reinforce momentum at key milestones.
Future AI Roadmap
Once the core programmes are proven at scale, SemaPen’s next wave of AI will turn great into groundbreaking.
Generative meal plans that respect culture and budget; computer‑vision food logging; predictive “early‑warning” relapse models; digital‑twin simulations; an LLM‑powered learning coach; voice‑first accessibility; AR nutrient overlays; a behavioural‑economics engine that fine‑tunes rewards; and federated learning that builds evidence without exposing patient data.
Every model is designed for NHS‑grade governance: transparent, explainable and switched on only when commissioners are ready—so innovation never outpaces trust.
| Theme | AI Idea | Why it’s Powerful (and NHS‑friendly) |
|---|---|---|
| Hyper‑personal nutrition | Dynamic meal suggestions – a generative model that proposes recipes and supermarket basket lists based on the user’s biometric trends, cultural preferences and budget. | Goes beyond static meal plans; drives day‑by‑day adherence while tackling cost‑of‑living barriers. |
| Predictive safety net | Early‑warning relapse model – combines weight trajectory, app usage patterns and sentiment in messages to flag who’s likely to stall or regain. | Enables “right‑time” human outreach, saving clinician hours and preventing expensive escalation to Tier 3 services. |
| Computer‑vision food logging | Shot‑to‑macro photo analysis that estimates portion size and nutrient breakdown. | Removes the tedium of manual logging yet keeps data quality high for outcomes reporting. |
| Conversational learning coach | LLM‑powered chat interface that quizzes users, answers questions in plain English and adapts Academy lessons to their knowledge gaps. | Boosts engagement without scheduling more webinars or live Q&A sessions. |
| Digital‑twin simulations | Individual “what‑if” models that show how weight, HbA1c and cardiovascular risk shift under different scenarios (e.g., +2 kg regain, drug tapering, pregnancy). | Makes consequences tangible, motivating adherence and supporting shared decision‑making with clinicians. |
| Federated learning for research | On‑device models train locally; only anonymised gradients are aggregated. | Generates real‑world evidence at scale while meeting stringent NHS Information Governance rules. |
| Augmented reality (AR) habit prompts | AR overlays that visualise sugar or fat content on a plate or supermarket shelf through the phone camera. | Turns abstract nutrition advice into an at‑the‑moment behaviour nudge. |
| Voice‑first accessibility | Voice‑enabled logging and coaching for users with visual impairments or low digital literacy, built on a domain‑tuned speech model. | Widens inclusion and meets NHS accessibility standards. |
| Behavioural economics engine | Reinforcement‑learning algorithm that tweaks reward schedules (badges, streak lengths, social prompts) in real time to maximise long‑term retention. | Keeps the gamification fresh and evidence‑based, reducing churn. |
| AI‑assisted MDT triage (optional) | When clinically acceptable, a rules‑plus‑LLM system could summarise user‑reported symptoms and draft clinician notes. | Cuts admin for dietitians and doctors; frees time for complex cases—but can be toggled off if policy shifts. |